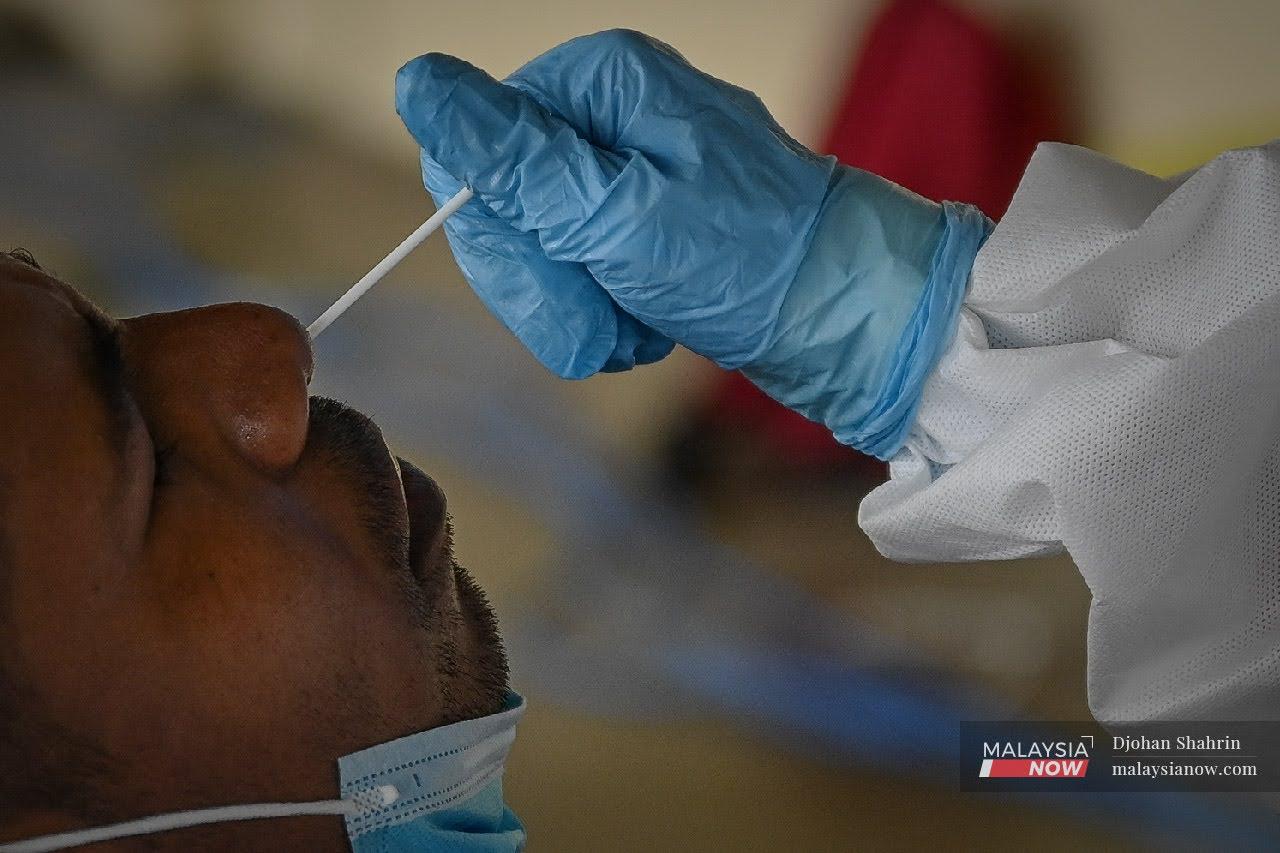
Are bad Covid test practices churning out false positive cases?
While only the authorities working together with independent parties and the scientific community can verify these probabilities, so far we have no reason to assume the worst.
Just In
The reverse transcription polymerase chain reaction (RT-PCR) is the gold standard for Covid-19 testing, but there have been some concerns about using RT-PCR with high-cycle protocol which could be giving rise to false positive results.
Even if this proves to be the case for RT-PCR machines, the overall impact of false positives is likely to be minimal given Malaysia’s epidemiological status and the overall practice of our health authorities in managing Covid-19.
To understand what this is about, let’s have a look at some basic concepts regarding how RT-PCR works.
Viruses carry in them genetic material in the form of sequences that are unique to it which we can use for identification. In general, PCR amplifies (or replicates) specific parts of a viral gene sequence (target genes). It replicates these target gene sequences in “cycles” whereby after each cycle, the number of gene replicates increase exponentially.
This is done so that we have enough genetic material to be detected. To detect these replicates, “probes” are added that will attach to these replicated genetic sequences. Under a certain type of light, these probes emit light back to the sensor. A stronger re-emitted light from the sample indicates more replicates and vice versa.
The minimum light intensity detectable is the “detection limit”. The number of cycles needed by the PCR machine to amplify the target genetic sequence to the detectable limit is known as the cycle threshold or Ct.
As pointed by Jonathan Jarry from the Office of Science and Society of McGill University, a high Ct risks reducing the “specificity” of the test. No technology is 100% perfect and functions perfectly all the time, and running high Ct could cause similar genetic sequences in the mix to be replicated. It’s amplifying irrelevant background noise, so to speak. This gives a false positive result.
So, there is worry that health authorities could be producing false positive cases if they are running high Ct – meaning, people get positive test results despite not actually being infected. But we cannot answer this by looking at the Ct value alone.
According to the Centers for Disease Control and Prevention (CDC), positive predictive value (PPV) is the likelihood of a person with a positive test result to most likely be infected.
Based on the CDC, PPV is greatly impacted by two major factors: pretest probability and test specificity. The higher the pretest probability and the specificity of a test, the lower the false-positive rate and the higher the PPV.
So the question is, have the authorities tested people with high pretest probability using high specify tests?
Let’s start with pretest probability. According to the CDC, pretest probability is based on epidemiological circumstances such disease prevalence in the population as well as clinical information such as symptoms and patient history of close contacts of the person being tested. The more prevalent a disease is in a population and the more clinical observations there are indicating illness, the higher the pretest probability.
Malaysia is obviously not in a situation of low disease prevalence and the health ministry’s guidelines to assess if a person fulfils the criteria for a suspected case include robust clinical and epidemiological criteria. These guidelines have been outlined by experts in the field and we have no evidence to say that these guidelines are insufficient or that that they have not been properly followed. In this case, pretest probability should be high.
According to Public Health Ontario (PHO) Laboratory, in general the PPV is “excellent” for Covid-19 PCR tests coming from people with high pretest probability, with PPV of almost 100%. Meaning, almost all of the people who test positive are really infected with the virus. The test by PHO Laboratory may use a different test kit under different circumstances and in a different place, but the impact on high pretest probability on reducing likelihood of false positives remains true.
Therefore, we are left with the second part of question: are the RT-PCR tests conducted on these suspected cases reliable? Are we using Ct values that are too high, causing the specificity to be questionable?
Going back to how the PCR works, Ct value is relative to the amount of genetic material the PCR test started with. If the test started with many samples of the virus gene (high viral load), its Ct will be low because it doesn’t need as many cycles to amplify it to amounts that can be detected. Conversely, if the Ct is high then it’s because the initial viral load is low and the RT-PCR takes many more cycles to produce enough replicated target sequences to be detected.
As you can see, the “reported” Ct is relative, not a value to be arbitrarily set. There are guidelines that have been set by the manufacturers of RT-PCR machines and kits which have to be followed by laboratory technicians. The World Health Organization (WHO) Information Notice dated Dec 20 regarding the interpretation of PCR test results does not contradict these in that any manual adjustments must be according to manufacturer’s recommendations.
The notice from WHO also recommends the reporting of Ct values, but emphasises that the result interpretation should be in consideration of various factors. This in line with the fact that the Ct value by itself doesn’t tell you much, and that PPV is affected by other factors as discussed before.
Therefore, the relevancy of the question may not be so much on the reported Ct, but more on the “cut-off” Ct values by manufacturers.
As reported by Kim Schive at MIT Medical, the healthcare arm of the Massachusetts Institute of Technology, MIT uses 40 cycles as the cut-off value. This means that a test result is deemed negative if the target virus sequence isn’t detected by the time it reaches 40 cycles, and positive if is detected within 40 cycles or less.
According to Public Health England, an executive agency of the Department of Health and Social Care in the UK, “a typical RT-PCR assay will have a maximum of 40 thermal cycles”.
Looking at the above two sources, it’s possible that a relatively high Ct cut-off value is being practised. As pointed out earlier, running at high Ct could run the risk of “noise amplification”, generating false positives.
Schive reported a similar view shared by associate medical director at MIT Shawn Ferullo who was quoted as saying: “I do believe the test (referring MIT 40-cycle test protocol) may be identifying some sub-clinical cases, but based on our current understanding of the virus, we’d rather err on the side of caution than put our community at risk.”
But even if the Ct cut-off value has been higher than ideal, we have to remember that PPV is also contributed by pretest probability, which as discussed above can greatly reduce the chance of false positives if done correctly.
Based on PHO Laboratory data as of Aug 15, 2020, there were 30 occurrences of possible false positive Covid-19 results from over 850,000 tests, of which about 17,500 tests were positive cases. This shows a total false positivity rate of about 0.003%.
All in all, it is still a valid concern, especially if cases are high and the health infrastructure is overwhelmed, which is the case for Malaysia right now. We would be wasting precious resources if there were significant false positives. As discussed, this is unlikely to be the case – unless the authorities have not been following their own robust guidelines in combination with wildly erroneous test kits.
Ultimately, only the authorities working together with independent parties and the scientific community can verify these probabilities, but so far we have no reason to assume the worst.
Although the science behind PCR is not new, the novel coronavirus is, as the name implies, so the science relating to it, including test kits and equipment, are bound to see improvements and changes over time. There are existing procedures and regulatory bodies that ensure we only use equipment that is reliable – or as reliable as can be at any given point of time.
In Malaysia, laboratories have to report the Ct value to the Special Committee on Covid-19 Laboratory (JPKMCOVID-19) as part of the procedure to offer RT-PCR tests. All test kits are validated by the Institute for Medical Research (IMR) or National Public Health Laboratry (NPHL). Accredited laboratories also perform verification of the test method before offering the test.
Ameen Kamal is head of science and technology at independent think tank Emir Research.
The views expressed in this article are those of the author(s) and do not necessarily reflect the position of MalaysiaNow.
Subscribe to our newsletter
To be updated with all the latest news and analyses daily.